These creatures have evolved special “nanobodies” that may have an edge over human antibodies when it comes to developing a new treatment.
Source: Wired
Millions of years ago, some unknown common ancestor of today’s llamas, camels, and alpacas underwent an unusual genetic mutation. This evolutionary happenstance gave llamas and their kin a strange type of antibody that no other mammals have—which, surprisingly, could end up aiding in the fight against Covid-19. On Monday, in the journal Nature Structural & Molecular Biology, researchers from the Rosalind Franklin Institute and the University of Oxford reported the discovery of two llama antibodies, also called nanobodies, that could prevent the virus that causes Covid-19 from infecting human cells.
“These [nanobodies] can block—do block quite potently—the interaction between the virus and the human cell,” says Ray Owens, a professor of molecular biology at the University of Oxford and one of the study’s senior authors. “They basically neutralize the virus.”
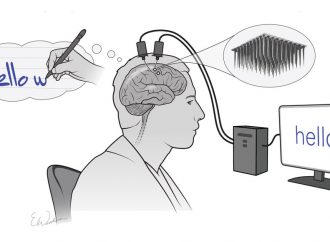
Like all antibodies, the nanobodies that Owens and his team developed have the ability to recognize and attach to a specific spot on a specific protein—in this case, the so-called spike proteins that cover the surface of the novel coronavirus. When these spikes latch onto ACE2, a protein that sits on the outside of many human cells, the coronavirus can enter and infect those cells. If, however, the spike proteins are blocked from attaching to ACE2, the virus will float around harmlessly, unable to invade.
Most species, including humans, make very similar antibodies. Typically, antibodies developed for medical treatments are first produced in lab animals such as rabbits, then isolated and genetically tweaked to more closely resemble human antibodies. But a few species, including llamas, their fellow camelids, and sharks, are antibody oddballs. These animals make nanobodies, so called because they are substantially smaller than their antibody cousins.
These tiny molecules have their own particular benefits. “Sometimes there might be a particular pocket that forms on the surface of a protein that’s recessed,” says Jason McLellan, an associate professor of molecular biosciences at the University of Texas at Austin who has also discovered a llama nanobody that blocks the spike protein from binding to ACE2. Larger antibodies, he says, “can’t bind inside that pocket.”
Even when they are used in exactly the same spots, nanobodies may have an edge over human antibodies. “They’re very stable,” Owens says. Unlike most antibodies, they maintain their shape in extreme environments, like the human stomach.
Given these advantages, nanobodies have been developed as treatments for diseases, and one has even been approved by the FDA as a cancer treatment. The tried-and-true method of developing nanobodies involves injecting a harmless chunk of the pathogen into a llama and waiting for the animal to mount an immune response. But inoculating a llama and extracting its nanobodies is a monthslong process, slow by the standards of Covid-19-era research. So Owens and his colleagues took a different tack.
They started with an enormous set of nanobodies that had previously been isolated from llamas. “We have a whole collection of different sequences with different binding potentials,” says Owens. They then used the spike protein to “fish out” any nanobodies that would attach to it. This strategy allowed them to quickly identify a nanobody that had potential against SARS-CoV-2.
Unfortunately, this nanobody didn’t attach to the protein tightly enough to effectively block the novel coronavirus from entering cells. So Owens and his team randomly mutated the region of the nanobody that connected with the spike protein, in hopes of creating a snugger fit. And they succeeded: In the presence of large enough quantities of one of these mutated nanobodies, SARS-CoV-2 was entirely incapable of entering human cells. “They literally can’t develop infection,” Owens says.Most Popular
McLellan and his team, who published their nanobody discovery in Cell in May, leveraged a different strategy. They were already developing a nanobody against SARS-CoV-1, the virus that caused the 2002–04 SARS epidemic; fortuitously, they found that this same nanobody proved effective against SARS-CoV-2.
While their nanobody has the advantage of being effective against multiple coronaviruses, the approach favored by Owens and his colleagues may have its own virtues. “Generally, in order to get breadth, you give up some potency or specificity against any one particular molecule,” McLellan says. “It’s a delicate balance.” Because Owens and his team optimized their nanobodies for use on SARS-CoV-2, they could prove more effective against it—though further research is needed.
Regardless of which type of nanobody comes out on top, two may be better than one for Covid-19 treatment. “These two nanobodies could be used simultaneously, to maybe generate an additive or synergistic effect,” McLellan says. Since the nanobodies discovered by each group attach to the spike protein at different spots, when used in concert they could team up to make it even harder for the spike to connect with ACE2.
These quick methods of adapting old nanobodies for new purposes are stopgap measures. Scientists are still waiting for the llamas that they have exposed to the spike protein to produce their own SARS-CoV-2 nanobodies from scratch: Both Owens and McLellan are currently working on such projects. “Using immunization, the natural immune system, to mature high affinity interactions obviously gives you the best binders,” Owens says.
In the meantime, both researchers hope that their nanobodies might prove to be effective treatments for people who are severely ill with Covid-19. While a patient’s immune system struggles to mount an adequate immune response, nanobodies and other types of antibodies could function as an emergency measure to prevent SARS-CoV-2 from entering more of their cells. The same rationale is behind treatments that involve injecting a patient with plasma from a Covid-19 survivor, but transfusions come with a risk of infection and depend on donations. Until a vaccine becomes available, some researchers believe antibody treatments could be used as short-term protection for health care workers and the families of patients.
One they reach the clinical stage, nanobodies might be more convenient to work with than other antibodies. Because they are so small, they can travel much more easily through body tissues, so they wouldn’t necessarily have to be injected into patients. “Potentially, they could be inhaled directly into the lung, where the respiratory infections are occurring,” says McLellan.
“They’re also much easier to make,” Owens says. Their small size means that they can be produced in bacteria—much more cheaply and more quickly than standard antibodies, which must be made in animal cells.
Jacob Glanville, president and CEO of Distributed Bio, a biotech company that is developing traditional antibodies for use against the novel coronavirus, believes that the ease of producing nanobodies is a material point in their favor. “I think that is a legitimate advantage,” he says. “I’m very concerned about the global capacity to produce CHO,” or Chinese hamster ovary cells, which are used to generate larger antibodies at scale.
In the long run, McLellan hopes that llama antibodies can help to prevent a pandemic like Covid-19 from ever happening again. “I think one of the next steps is to start trying to identify antibodies and nanobodies that can broadly bind and neutralize diverse coronaviruses,” McLleland says. “In the event there’s another coronavirus outbreak in the future, we might then already have the antibody immediately, from day one, that could work and neutralize the virus.”
Source: Wired






















Leave a Comment
You must be logged in to post a comment.