A man in France has regained some aspects of consciousness after being in a vegetative state for 15 years, after surgeons used a technique to stimulate his brain via a nerve in the neck.
The 35-year-old was diagnosed as being in a vegetative state – now referred to as “unresponsive wakefulness” – after a car accident in 2001.
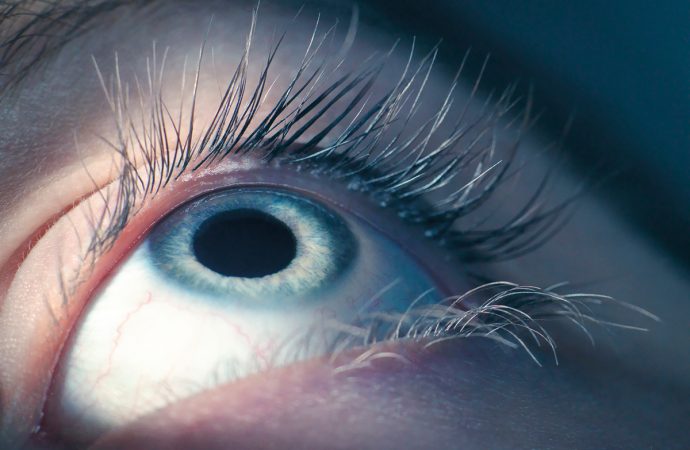
A person in this state might show involuntary movements, but has no awareness of self or their environment. Repeated tests over the years showed no improvement in the man’s condition.
That was until Angela Sirigu of the French National Centre for Scientific Research in Bron and her colleagues trialled a new technique that focused on the vagus nerve.
The vagus nerve runs from the brain to several areas of the body. It modulates the parasympathetic nervous system, which controls heart rate and lung function, among other processes.
It connects, directly or indirectly, to brain areas including the thalamus – a highly interconnected hub of neural activity, the amygdala, which regulates emotion, and the hippocampus, which is heavily involved in memories. The nerve also stimulates the locus coeruleus, the brain region that controls the release of brain chemicals involved in arousal and alertness.
Sirigu’s team hypothesised that stimulating the vagus nerve would increase activity in brain regions that could help the man regain consciousness. “I believe that’s what happened,” says Sirigu.
Constant stimulation
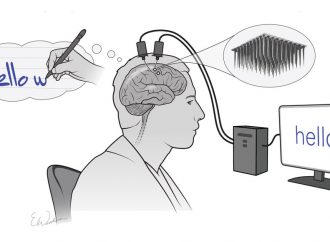
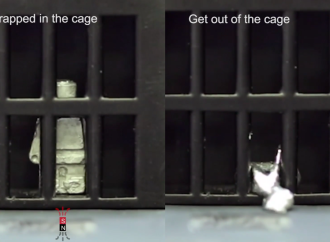
To test the idea, the team wrapped very thin electrodes around the vagus nerve in the man’s neck. He was monitored for a month before the nerve was stimulated. They then treated him continuously over six months. Each treatment involved 30 seconds of stimulation followed by 5 minutes of rest. The team started with an electrical current of 0.25 milliamperes, increasing by 0.25 mA a week up to 1.5 mA.
Clinicians regularly monitored changes in the man’s behaviour throughout the trial, while Sirigu’s team recorded EEG signals from the scalp before stimulation began and at points throughout the trial. They also scanned the man’s brain using positron emission tomography immediately after the electrodes were implanted and six months later.
As soon as the stimulation started, the man began to open his eyes more often. After a month, he began to track people around the room with his eyes. He was even able to respond to requests to turn his head from one side to the other. He also attempted to follow an instruction to smile.The team have not yet used these movements to ask him questions, such as whether he is in any pain.
His scores on the “coma recovery scale” suggested he could now be defined as being in a minimally conscious state – in which a person has partial conscious awareness.
The man has not regained the ability to talk or walk, which he is unlikely to do, given the large damage to his brain. The team are continuing to track his progress.
Brain stimulation
The behavioural changes, which stabilised after the first month of stimulation, were backed up by changes in brain activity. Many areas of the cortex showed increased activity after the stimulation. “We observed activity in those areas that were mostly targeted by the vagus nerve,” says Sirigu.
This included the parietal cortex. “This area is key for consciousness,” she says. People with lesions in the parietal cortex often show impaired consciousness.
Steven Laureys of the University of Liege in Belgium, who has worked extensively with people with impaired consciousness, is happy to see the results. “Clinicians for way too long have considered patients of unresponsive wakefulness as just waiting to die. And that is not true. There is some capacity for plasticity, and this is one other study showing that there can be changes,” says Laureys. “I’m convinced that vagus nerve stimulation is a potential new treatment.”
But he does think the clinicians should have done more to establish a better baseline before the treatment. The team tested the man three times over two months before stimulation began to establish that he was unresponsively wakeful. Laureys’s team has shown that accurate diagnosis requires five assessments within one to two weeks. “It’s known that these patients fluctuate,” says Laureys.
He cautions against generalising about the results. “We need to be careful. It’s not that we can now implant any patient and give them back consciousness. The challenge is to understand why this works. It will not work in all patients.”
Laureys would like to see randomised, controlled trials done at multiple centres, before claiming that the technique is ready for use in clinical settings. “We shouldn’t give false hope,” he says. “But we also shouldn’t give false despair.”
A difficult decision
The fate of people in a vegetative state remains a controversial subject. Just this week, the Court of Protection in England and Wales ruled that the families of people in a vegetative state no longer need the court’s permission to stop artificial feeding and let their loved one die. They can now do so if family and doctors agree it is in the patient’s best interests.
For now, Sirigu remains hopeful that their technique will work on others in a similar state. Her team is now studying more patients to see if the results can be replicated.
Source: New Scientist





















Leave a Comment
You must be logged in to post a comment.